I read Dr. Cifu’s article, “Please do not do that research”, which provocatively argues that some areas of biomedical research are no longer worth pursuing. His intent is clear: to encourage clinicians, overwhelmed by academic career pressures, to avoid studies whose results seem obvious or unlikely to change practice. I found the article to reflect a reductionist and centralized view of research.
I believe that decentralized exploration largely driven by curiosity is the backbone of disruptive and transformative discoveries. As such, opinionated pieces declaring entire fields “settled” strike a chord. I was challenged to provide my concrete thoughts on why.
So, I reply point-by-point to Dr. Cifu’s ten areas of research he suggests we should abandon.
Smoking
We do not need to learn anything else about the harms of smoking. No new data will change what we tell patients. Do not start smoking. If you smoke, stop.
According to WHO, ca. 1.25 billion people worldwide still smoke. While we know for sure that smoking is harmful, tobacco remains a major public health issue and a leading preventable cause of suffering and death. Unfortunately, we are very bad at persuading people to quit smoking.
Some smoking research areas that I believe are specifically interesting and relevant:
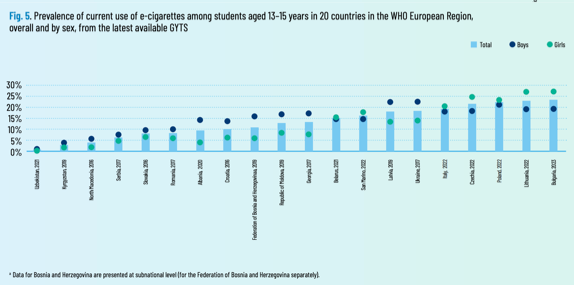
New trends emerge. E-cigarettes and vaping are becoming increasingly common.
The widepread opinion in the public is that the harms of vaping are less than those of conventional cigarette smoking [Edit: thanks to the comment by Joe Gitchell (https://substack.com/@joegitchell), I now learned that public opinion has shifted with most people considering e-cigarettes to be equally or more harmful than conventional cigarettes]. Is this true? We are far from being able to answer that. Relevant for patients? Example: a patient comes after a stroke to their doctor with the argument: “I tried hard to quit smoking last year after my stroke. I failed every single time. I now found that vaping helps me smoke fewer cigarettes.” What should we reply to this patient? Should we encourage them?
Why are some people more predisposed to smoking addiction? Figuring out the biology underlying addiction can help us identify novel therapeutic targets and subsequently drugs to help patients quit smoking more efficiently. Genetic studies asking this question already point to promising targets.
While smoking is detrimental for most diseases, there are noteworthy exceptions. There is a very robust inverse association between smoking and risk of Parkinson’s disease that we barely understand. Given the lack of disease-modifying therapies for Parkinson’s disease shouldn’t we investigate one of the few apparently “protective” risk factors more thoroughly?
There are really a lot of examples here. Guidelines for most diseases are still informed by ongoing studies. For example, the latest guidelines for secondary stroke prevention by the AHA (2021) were largely informed by observational and interventional studies on smoking performed after 2015.
The same guidelines highlight some research gaps:
Future research in established stroke or TIA is required for the following:
…
• To further develop stroke registries to address knowledge gaps in recurrent stroke, including the contribution of continued smoking (currently limited to Asian and older populations), heavy alcohol consumption (currently lacking), and substance use (currently lacking).
• To identify the longer-term cardiovascular consequences of newer tobacco products, for example, electronic nicotine delivery systems (electronic cigarettes/vaping), which are not currently known.
• To consider the dual use of electronic nicotine delivery systems (electronic cigarettes/vaping) with combustible cigarettes in studies relating to the longer-term cardiovascular consequences, including stroke and recurrent stroke.
• To examine the association between ischemic stroke and recurrent stroke and therapeutic cannabis use (currently unknown) and recreational cannabis use (currently limited to young adults only and using surveillance data).
Exercise
We do not need to learn anything else about exercise. It is good for you. You should be active, as active as possible. There may be subtle differences in the benefits of exercise based on timing, degree, and strategy, but for nearly everyone, you just need to find something you enjoy and can make part of your daily routine.
This is clearly reductionist thinking. The fact that we know of an intervention that works so well, doesn’t mean that the field has nothing left to expore. On the contrary, it is exactly its effectiveness, where countless opportunities for discovery are hidden.
How does exercise confer protection against disease? What are the underlying mechanisms? Understanding those can lead to a better understanding of disease and aging mechanisms. This can lead to development of novel therapeutics or even alternative preventive or disease-modifying approaches for individuals unable to exercise.
Similar to nutrition (see below), exercise is hard to measure. There’s a lot of noise due to self-report. People forget (willingly or unwillingly) how many times they went jogging per week in the last year. Or how many times they hit the gym. Or when they started going to the gym. Or how long they exercised. Better phenotyping of exercise behaviors using digital approaches, such as wearables or smartphone apps to objectively quantify exercise patterns over long periods of time is a very fascinating field of research. This can trigger a new generation of exercise studies with much more accurate assessment of the effects of exercise.
Are we really sure that there are only subtle differences between types of exercise? Is the same intensity or type of exercise the same for different groups of people? Should an 18-year old aiming for lifelong disease prevention do the same type of exercise as an 85-year old stroke survivor with hemiparesis?
Why do some people respond better to exercise than others? What drives VO2max gains, what drives muscle strength? We now have newer techniques for capturing physiologic effects at scale in large cohorts.
Any negative aspects of exercise? Are long-distance runners at risk of knee osteoarthritis?
The fact that an intervention is “good” doesn’t mean that we “do not need to learn anything else” about it. Magnitude of effect, heterogeneity of response, deeper understanding of its mechanistic effects are all extremely important. Exercise is an exciting field with loads of opportunities.
Nutrition
We never need another observational study about nutrition. Between confounding and the vibration of effects, these studies will not show us anything of importance. It would be wonderful if we could find diets that will make us healthier; these studies will not do it.
Nutritional epidemiology has (for very valid reasons) become the poster child for how confounding can bias observational research. Still, the fact that we currently lack perfect tools to understand the effects of nutrition on human health, doesn’t mean that we should abandon nutritional research. On the contrary, several topics remain highly relevant:
Addressing measurement error, we now have image-based food-logging apps that allow for accurate assessment of nutritional patterns. This generates very complicated datasets with an abundance of datapoints that will by themsleves allow the generation of novel quantitative methods to assess nutrition as an exposure.
Similarly, re-analyses of trial data have allowed the development of omics-based signatures (e.g. lipidomics, microbiomics or metabolomics) of adherence to specific diets. These signatures represent a new generation of tools to perform observational nutritional research with higher accuracy.
Plant-based diets are more common than ever before. We clearly lack an understanding of their long-term effects. What are the longest available studies? Like 20 years? Shouldn’t this be investigated further?
Protein intake? There is a huge ongoing discussion about protein intake needs. Should the scientific community remain far from it? Should we leave this discussion to podcast and social media protein promoters?
I believe that nutritional research will enter its golden era in the near future. There is clearly more interest from the public and we now have way better tools of more accurately assessing dietary trajectories reliably. Of course, there is confounding. There always are problems. But this is exactly where opportunities exist.
Dementia
We never need another observational study on dementia prevention. The same arguments apply here as for observational nutrition studies. The best way to prevent dementia is to have good genes and maintain a healthy lifestyle. If we want data on dementia prevention, start an RCT. If an RCT can’t be done because the intervention could not be maintained for 10 years, well, there is your answer.
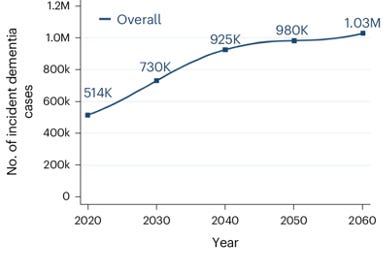
Dementia is going to be one of the major public health problems of the 21st century. Whoever needs confirmation about that should just look at the data.
Arguing that dementia research should be restricted to RCTs, like RCTs appear out of thin air, makes no sense. “Have good genes and maintain a healthy lifestyle”. Really? Couldn’t we say the same about heart disease, stroke, and diabetes already 60 years ago? Should we have stopped there? We wouldn’t have any statins, many blood pressure lowering interventions, PCSK9 inhibitors, SGLT2 inhibitors, GLP1 receptor agonists, etc.. A lot of observational research about the role of LDL and HDL cholesterol, blood pressure, glucose levels, BMI and so on preceded the trials.
Some interesting areas of dementia research:
Are there early diagnostic signatures of neurodegenerative diseases that we could use to identify candidates for treatment trials? There are beautiful initiatives for omics and neuroimaging markers.
What is the natural history of dementia? Is it indeed the case that neurodegeneration starts decades before the first clinical symptoms? How many years is the typical duration of mild cognitive impairment before transitioning to dementia?
How can we separate the different pathologies related to dementia (e.g. Alzheimer’s, vascular, frontotemporal) in vivo? Do biomarkers of these pathologies relate to clinical trajectories?
Who would be best candidates for emerging disease-modifying therapies?
What should we tell patients with subjective cognitive complaints or mild cognitive impairment that come to our memory clinics? Patients have questions like “do I need to take care of my finances?”, “will I lose my mind in the next two years?”, “should I spend more time with my family”? On the basis of which numbers should we inform them about their prognosis, if not based on observational research?
Genetic risk is also a beautiful area, especially in dementia. Is there anything that can mitigate risk in APOE ε4 carriers? Should we design prevention trials for these individuals? If yes, with which intervention? What does observational research suggest?
If anything, most people agree that, for the magnitude of the problem, dementia is considered largely underfunded. So, please, engage into research in dementia.
Loneliness
Please, no more studies about the health effects of loneliness. Loneliness is miserable, but we will never know if it makes people less healthy because it is impossible to get non-confounded data from observational studies — are you sick because you are lonely, or are you lonely because you are sick? I wish fewer people were lonely. If you have some ideas about how to achieve this, study that.
Once again, the argument that we aren’t good at studying a specific topic isn’t an argument for abandoning research on this topic entirely.
Reverse causation could be largely handled in studies with very long follow-ups (>20 years) and we increasingly have such cohorts.
Methods for objectively quantifying social networks with social network analysis offer a great opportunity for interesting research.
Race, gender, or age of physicians
We can do without studies that look at outcomes correlated with the race, gender, or age of physicians. First, like many of the topics above, most of these studies show small effect sizes and are likely compromised by residual confounding. Most importantly, what are you going to do with the data? No more male physicians? All doctors over 40 have to work with a doctor under 30? Only race-concordant doctor-patient relationships are allowed?
Not every phenomenon needs to be studied in the face of a downstream massive and highly effective intervention. Such observations are the first step towards understanding some of the biases or inefficiencies of our healthcare systems. Potential solutions don’t need to be as radical as “no more male physicians”. If indeed, women practice on average better, we can detect which practice patterns drive outcome differences, so that we improve training for all physicians.
Also, there are other practical consequences. Is there a need for continuing medical education or not? Should a fix retirement age be implemented for specific specialties (e.g. surgery or anestheesiology?). How should policies be informed if not by such studies?
Socioeconomic status
Health outcomes by socioeconomic status. Being poor, in almost any country, is terrible for your health. So, just as smoking (which poverty is compared to in the source of the figure) is harmful, we don’t need data to tell us that poverty is bad for us. One more study will not embarrass us into finally working to decrease economic inequality. Use the money that funds these studies to do something about the poverty (or to study interventions to reduce poverty).
I agree that poverty and economic inequality are major (probably the main) drivers of human disease disparities. Whoever had the chance to ever run a survival analysis with socioeconomic status as exposure can guarantee that it splits the curves for any health outcome better than any other variable in any dataset. But does this mean that we don’t need to study it further? Again, not.
Of course, the ideal solution would be to solve poverty. That’s what a real Marxist would argue. Good luck with that.
A more pragmatic approach is to dissect the effects of low SES on health outcomes. For example: Why does poverty drive worse colon cancer prognosis? Is it lower access to preventive measures (e.g. colonoscopy) leading to delayed diagnosis? Delayed recognition despite timely presentation to a physician? Worse treatment options due to insurance inequalities? The solution to each of these problems is different and more granular than “solve poverty”.
Medical education
Do not study “innovations in medical education.” These studies almost never give us usable data because it is nearly impossible to measure an outcome.1 How do you measure the “quality of a doctor.” There is one medical education study worth reading, a case-control study with an ingenious, objective outcome.
Once again, the same pattern: we have bad ways of measuring X, let’s abandon researching this topic. Doctors should remain humble and not forget that medical error and complications to our interventions are a serious source of harm in healthcare settings. I’m not very familiar with medical education research, but I can think of at least some good outcomes (e.g. complication rates for surgeons or procedure success rates for any interventionalist).
Vitamin D
Please, no more studies of any kind on the health effects of vitamin D. We already have thousands of observational and experimental studies on vitamin D supplementation. If your vitamin D is normal, more almost certainly does nothing; if it does has an effect, it is minuscule. Enough is enough!
I largely agree that vitamin D megatrials have provided no evidence for benefit of vitamin D supplementation. Still, as always, there are open topics that make further research necessary:
We shouldn’t forget that vitamin D supplementation is recommended for all infants for prevention of rickets. This is a massive intervention that needs to be periodically reassessed.
There is quite consistent research suggesting a role of vitamin D in multiple sclerosis. The interventional trials haven’t come to a consensus yet about whether supplementation helps to prevent relapses, but there are some interesting positive data for patients with clinically isolated syndrome.
Seed oils
And last but not least, let’s refrain from conducting any further observational studies of seed oils. I suppose this is a corollary to #3, but it is talked about enough to warrant its own bullet. Not only will we never get clean data, but no matter how good the data is, you will never convince the enemies of seed oils of anything.
I will not comment on this, as I have never read a single study focusing on seed oils.
Closing remarks
Dr. Cifu’s view of research is that of a one-shot game. Answer a question, then move on to making a difference. You can’t answer the question, put your effort elsewhere. In reality, science is very iterative. Areas that seem settled may yield new insights and interventions. And challenges in unsettled areas often get overcome through innovative technologies that open whole new fields of research. While I understand the need to centrally define research priorities and allocate resources accordingly, completely disregarding entire areas of research is short-sighted. Authority figures in science or medicine who argue, “you shouldn’t do that research because we think it’s bad,” shouldn’t forget that transformative discoveries and transferrable innovations can emerge from any field. Curiosity at an individual level is the key driver. Declaring research areas closed risks closes doors on discoveries we don’t yet know we need.
As a disclaimer, I’m not an expert in any of the fields above (I have previously conducted research on vascular contributions to dementia). These are just my high-level thoughts. Please comment, add, or correct me if I’m wrong.



I enjoyed your thoughtful response to Dr. Cifu’s tongue-in-cheek post. I think there is good wisdom in the two taken together. And, they were both fun to read. Thank you.
Highly gratified that SM is the rare source of well thought out opposing opinions: both of which in this case have merit. Well worth my monthly subscription.